Table of Contents
Think about a hospital where doctors pull up patient charts in seconds, nurses update records on the go, and admins track billing without mix-ups. That smooth flow saves lives and cuts costs. It comes from picking the right EHR software. Hospitals today face packed wards, tight budgets, and strict rules. Good EHR handles all that. It stores patient info safely, shares data across teams, and spots health trends early. The best systems boost care quality and staff work. They fit big city hospitals or small rural ones. This post looks at top choices to help leaders choose well. Stick around to see which ones stand out and why they matter now.
Join Entri’s Hospital Administration Course
Introduction: Why EHR Matters in Hospitals
Hospitals run on quick info. EHR replaces old paper files with digital ones. Doctors see full patient histories right away. This cuts errors like wrong meds or missed allergies. Nurses spend less time on paperwork and more on care. Admins handle billing faster and get paid sooner. Patients gain too. They access their own records through portals and book visits online. Security stays tight with encrypted data and access controls. Rules like HIPAA demand that. Without strong EHR, hospitals lag. Delays happen. Costs rise. Care suffers. Top systems fix these issues. They link with labs, pharmacies, and other hospitals. Data flows free but safe. Analytics tools predict outbreaks or spot high-risk patients. Mobile apps let staff work from anywhere. Training staff takes time at first but pays off long term. Hospitals with good EHR see shorter stays and happier teams. The switch brings challenges like setup costs but leads to big savings. Leaders pick EHR to stay ahead. It turns data into better health outcomes. Now more than ever, with rising patient loads, EHR drives success.
Top EHR Software for Hospitals
TruBridge focuses on revenue and data insights.
Contract management handles deals with suppliers. Performance dashboards show key metrics at a glance. Electronic records keep patient info current. Pros come from personalized fits and collection boosts. Cons involve longer setup for custom parts. Costs hover near $500 monthly. It works well for hospitals needing financial tools alongside care. MEDHOST excels in emergency departments. Bed management tracks open spots in real time. Billing handles claims fast. Patient portals give access to discharge plans. Pros show in tailored doctor tools and outcome gains. Cons mention minor tech glitches at times. Pricing lands around $1,000 monthly. Hospitals use it for multi-site integration and secure exchanges. WellSky targets rehab and post-acute care. Care coordination links teams across settings. Compliance tools meet rules without hassle. Billing integrates with pharmacy modules. Pros include user-friendly templates and quick support. Cons note room for better reports. Fees start at $500 per provider. It fits hospitals with rehab wings for smooth transitions.
NextGen Enterprise stands out for engagement.
All-in-one portals connect patients and staff. Specialty designs fit value-based care. Mobile access works on phones. Security blocks threats. Pros cover easy billing and custom flows. Cons include spotty support at times. Monthly costs begin at $299 per provider. Hospitals like its population health focus for chronic cases. AthenaOne brings cloud power. Telehealth joins video calls direct in the system. Revenue management cuts denials. Reporting pulls insights fast. Pros lie in auto workflows and marketplace links. Cons point to training needs. Pricing bases on collections for flexibility. It serves hospital networks with care gap spots. Veradigm offers visit templates and telehealth built in. Medication tools manage scripts safely. Care plans set goals clear. Pros include one-click ease and data pulls. Cons note slow support responses. Pricing starts at $149 monthly for some parts. Hospitals choose it for multi-location flexibility. EClinicalWorks adds population tools. Scheduling books slots quick. Patient portals send reminders. Clinical support aids decisions. Pros show in auto tasks and data search. Cons involve learning curves. Costs run $449 monthly for core EHR. It helps hospitals coordinate across specialties.
Praxis EMR uses AI for docs.
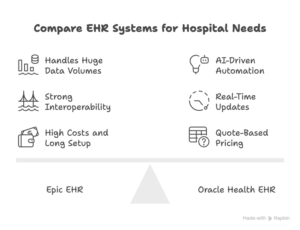
Template-free design adapts to users. Billing codes revenue right. Analytics meet compliance. Pros cover peer knowledge shares and order changes. Cons limit to integrations. Fees start at $219 monthly over time. Hospitals pick it for new or specialty setups. These systems share common strengths like data safety and mobile use. Each brings unique perks. Epic leads for big operations with its network reach. Oracle shines in AI smarts for risks. Meditech fits budget-conscious mid-size spots. TruBridge boosts finances. MEDHOST speeds emergency flows. WellSky smooths rehab links. NextGen engages patients deep. AthenaOne flexes with telehealth. Veradigm customizes visits. EClinicalWorks manages groups. Praxis learns user styles. Costs vary but return through efficiency gains. Hospitals weigh size, budget, and needs when choosing. Demos and trials show real fit. User reviews guide too. Top picks reduce errors and speed care. They prepare hospitals for future demands like more telehealth or AI aids.
Key Hospital EHR Features to Compare
Hospitals compare EHR on several key points.
Interoperability ranks high. It lets systems share data with labs or other hospitals. Good ones use standards like FHIR for easy links. This cuts repeat tests and speeds diagnoses. Security comes next. Encryption protects patient info. Access logs track who sees what. Compliance with HIPAA avoids fines. Look for audit tools that flag odd activity. User interface matters for quick adoption. Simple screens reduce clicks. Custom dashboards show vital stats first. Training modules help staff learn fast. Mobile access allows updates from bedsides. Apps work on tablets or phones. This fits busy shifts. Analytics pull insights from data. Reports spot trends like readmission rates. Predictive tools warn of risks. This guides better resource use.
Integration with other tools boosts value.
EHR links to billing software for clean claims. Pharmacy ties check drug interactions. Device connects pull vitals direct. Cost breaks down to setup, monthly fees, and add-ons. Some charge per user. Others base on revenue. Factor in training and support costs. Customization lets hospitals tweak workflows. Templates fit specialties like oncology. Rules automate alerts. Patient portals engage people. They view labs, pay bills, and message teams. This cuts calls and boosts satisfaction. Support quality seals the deal. 24/7 help fixes issues fast. Updates add new features without downtime. Scalability grows with the hospital. Cloud options expand easy. On-site setups suit some security needs. Compare downtime risks too. Reliable systems back up data often. Redundancy keeps access during outages.
Ease of use cuts training time.
Intuitive designs mimic paper charts at first. Voice input speeds notes. Compliance features track rules changes. Alerts remind of required fields. Revenue tools code visits right. They flag denials early. This keeps cash flowing. Reporting meets board needs. Dashboards show key metrics live. Export options feed other apps. Telehealth embeds video in records. This fits remote consults. AI adds smart notes and suggestions. It pulls data from past cases. Hospitals check vendor stability. Long-term players offer steady updates. User groups share tips. Trials test fit before buy. References from similar hospitals guide choices. These features make EHR a smart pick. They turn data into action. Hospitals gain from better care and lower costs.
Join Entri’s Hospital Administration Course
Conclusion
Top EHR software transforms hospitals. It streamlines work and lifts care. Systems like Epic and Oracle lead with strong tools. They fit needs from small clinics to big networks. Key features like security and analytics make the difference. Compare them to find the right match. Good EHR cuts errors and saves time. It prepares for busy days ahead. Leaders see returns in happy patients and teams. Pick one now to stay strong.
Frequently Asked Questions
What makes EHR software essential for hospitals?
EHR software serves as the central hub for all patient information in a hospital. It stores medical histories, lab results, medications, allergies, and treatment plans in one digital place. Doctors access this data instantly during rounds or emergencies. This quick access reduces mistakes like prescribing drugs that cause reactions. Nurses update vital signs and notes right away, which keeps the whole team informed. Billing staff pull accurate codes for claims, leading to faster payments and fewer denials. Hospitals meet legal rules on data privacy and reporting through built-in tools. Without EHR, paper charts get lost or misread, causing delays in care. Good systems also connect to outside labs or pharmacies for automatic updates. Patient portals let people see their own records and communicate with staff. This cuts phone calls and boosts satisfaction. Analytics spot patterns, such as rising infection rates, so leaders act early. Mobile access means updates happen at the bedside. Overall, EHR improves safety, speeds work, and lowers costs through better efficiency. Hospitals that choose strong EHR see shorter patient stays and higher staff morale.
Which EHR system works best for large hospitals?
Large hospitals often choose Epic or Oracle Health for their scale and depth. Epic holds the biggest share in inpatient settings because it handles complex networks well. It supports multiple sites, tracks every detail from admission to discharge, and offers strong tools for revenue and population health. Oracle Health, once Cerner, fits enterprise needs with its AI features that flag risks and automate notes. Both systems integrate deeply with other hospital tools like imaging or pharmacy software. They provide robust security and compliance features to meet strict standards. Setup takes time and money, but the payoff comes in smooth operations across big teams. Smaller or mid-size hospitals may find them too heavy. For very large systems, these two lead because they grow with the organization and handle massive data loads without slowing down. User reviews praise their reliability in high-volume environments like teaching hospitals or multi-state networks.
How much does hospital EHR software typically cost?
Hospital EHR costs vary widely based on size, features, and vendor. Epic and Oracle Health often run into millions for large setups, with ongoing fees per user or based on revenue. Smaller hospitals might pay $500 to $1,000 per month per provider for systems like Meditech or TruBridge. Cloud options keep upfront costs lower than on-site servers. Add-ons like telehealth or advanced analytics increase the price. Implementation includes training, data migration, and customization, which can add hundreds of thousands. Many vendors charge setup fees plus monthly subscriptions. Public hospitals sometimes get grants to offset costs. Return on investment shows through fewer errors, faster billing, and better reimbursements. Compare total cost over five years, including support and updates. Quotes depend on hospital beds, users, and needed modules. Always ask for breakdowns to avoid surprises.
What key features should hospitals look for in an EHR?
Hospitals need interoperability to share data with labs, pharmacies, and other providers without hassle. Strong security protects sensitive info with encryption and access logs. User-friendly interfaces reduce training time and errors. Mobile access lets staff update records from anywhere. Analytics tools pull reports on trends like readmissions or resource use. Patient portals engage people by letting them view results and message teams. Billing integration codes visits correctly and flags issues early. Clinical decision support offers alerts for allergies or best practices. Telehealth built in supports remote consults. Customization fits workflows for specialties like emergency or surgery. Reliable support provides quick help during issues. Scalability grows as the hospital expands. Cloud deployment eases updates and backups. These features ensure safe, efficient care and meet regulations.
How long does it take to implement an EHR in a hospital?
Implementation time ranges from six months to two years depending on hospital size and system choice. Small to mid-size hospitals often finish in six to twelve months with cloud systems like Meditech. Large networks with Epic or Oracle Health take twelve to twenty-four months due to complex data migration and customization. Steps include planning, training staff, testing, and going live. Data transfer from old systems takes the most time. Training ensures everyone knows how to use it safely. Phased rollouts, like starting in one department, cut risks. Vendors provide project managers to guide the process. Downtime planning keeps care running during switchover. Good preparation shortens the timeline. Hospitals that involve staff early see smoother adoption. Post-go-live support fixes issues fast. Full benefits appear after teams adjust.
Can small or rural hospitals afford good EHR software?
Small and rural hospitals can afford solid EHR options that fit their scale. Systems like Meditech, TruBridge, or MEDHOST offer cloud versions with lower upfront costs. Monthly fees start around $500 per provider, often with grants or subsidies for rural areas. These provide core features like records, billing, and patient portals without needing huge IT teams. Interoperability connects to larger networks for specialist consults. Vendors tailor pricing for smaller volumes. Cloud setup avoids expensive servers. Training comes included or low-cost. Rural hospitals gain from telehealth modules for remote care. Many see quick returns through better reimbursements and fewer errors. Government programs help cover costs in underserved spots. These systems scale as needs grow without breaking budgets.
How does EHR improve patient safety in hospitals?
EHR boosts patient safety by making information clear and available instantly. Allergy alerts pop up before meds get ordered. Drug interaction checks prevent harmful combinations. Barcoding scans confirm right patient and dose. Full histories show past issues like surgeries or conditions. Real-time updates keep teams current on changes. Clinical rules guide best practices, like sepsis protocols. Legible notes replace hard-to-read handwriting. Audit trails track who accessed records. Secure sharing avoids lost test results. Analytics spot safety trends early. Patient portals remind people of meds or follow-ups. Fewer errors lead to shorter stays and better outcomes. Hospitals report drops in mistakes after strong EHR adoption. It creates a safer environment for everyone.
What role does interoperability play in choosing hospital EHR?
Interoperability allows the EHR to exchange data with other systems smoothly. Hospitals need this to pull lab results, send prescriptions, or share records with referring doctors. Standards like FHIR make connections easier. Good interoperability cuts repeat tests and speeds decisions. It supports care coordination across providers. Vendors with strong links to common tools win here. Epic and Oracle Health excel in this area for large networks. Smaller systems integrate well too. Without it, data silos cause delays and risks. Check vendor certifications and real-world examples during demos. Strong interoperability future-proofs the system as health networks grow.