Table of Contents
Try this mental image: a patient in a distant village talking with a specialist hundreds of miles away, face-to-face. No travel, no waiting, just helpful guidance and prompt care. This kind of scenario happens every day, and its vector is telemedicine software. This software allows healthcare professionals to serve more patients more efficiently, spending less while maintaining a high level of safety. The rise of remote visits was swift and came from recent years. This phenomenon maintains its grip on our busy lifestyles and healthcare needs. To make such remote visits feel natural, the software is good. The software includes scheduling, payments, and chat. The benefits to healthcare institutions lie in the software, which suits the needs of healthcare workers. This article presents what telemedicine software is, the key aspects to look for, the top telemedicine software for healthcare professionals, the future changes. Continue reading to get the right software to increase your reach and ease your efforts.
Join Entri’s Hospital Administration Course
Introduction: What Is Telemedicine Software?
Telemedicine software lets healthcare providers deliver care from a distance. It uses video calls, messaging, and data sharing over the internet. Doctors see patients without in-person visits. This works for check-ups, follow-ups, mental health talks, or urgent issues. Basic setups include a camera and screen for live talks. Advanced ones add file sharing, e-prescriptions, and payment links. Patients join from home on phones or computers. No special apps needed in many cases. Providers set up waiting rooms and control sessions. Software keeps talks private with strong encryption. It follows rules like HIPAA in the US. Many integrate with electronic health records for full patient views. Billing happens right in the platform. Reminders go out by text or email. This reduces no-shows. Rural patients gain access to experts they could never reach before. Urban ones save time on traffic and parking. Providers see more patients in less time. They cut overhead from office space.
Telemedicine software changes how care happens.
It makes health services available anytime, fits chronic conditions that need regular checks, helps during bad weather or illness spikes. Adoption rose sharply and stays high. Providers who use it report higher satisfaction. Patients like convenience and quick responses. The tool bridges gaps in healthcare delivery. It supports mental health talks without stigma. It aids second opinions fast. Hospitals use it for discharge follow-ups. Clinics add it to extend hours. Software evolves with better video quality and AI aids. It stands as a core part of modern care. Adoption rose sharply and stays high. Providers who use it report higher satisfaction. Patients like convenience and quick responses. The tool bridges gaps in healthcare delivery. It supports mental health talks without stigma. It aids second opinions fast. Hospitals use it for discharge follow-ups. Clinics add it to extend hours. Software evolves with better video quality and AI aids. It stands as a core part of modern care.
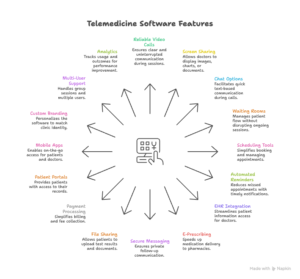
Key Features to Look for in Telemedicine Software
Best Telemedicine Software for Healthcare Providers
Doxy.me stands out for its simple design. It runs in any browser without downloads. Patients join with one click. Free plan offers unlimited visits with basic HIPAA compliance. Paid tiers add custom branding and group calls. Waiting rooms and chat keep things organized. Providers praise quick setup and low cost. It fits small clinics or solo doctors best. Teladoc Health provides full virtual care. It covers primary, urgent, and specialty needs. 24/7 access connects patients anytime. Integration with health plans streamlines billing. AI tools help triage cases. Large networks use it for broad reach. Amwell scales for hospitals and systems. It links with existing records and devices. Remote monitoring tracks vitals from home. Behavioral health and chronic care get strong support. Custom workflows fit different specialties. Mend focuses on ease for providers. It handles scheduling, payments, and reminders. Text and video keep communication smooth. Patient engagement tools boost satisfaction. Small to mid-size practices like its clean interface. VSee offers secure video with extras. It includes whiteboards for drawing and screen share. Group therapy sessions work well. HIPAA compliance stays tight. Clinics use it for mental health or family talks.
SimplePractice targets wellness and therapy providers.
It combines records, billing, and telehealth. Calendar syncs appointments. Secure messaging and portals engage clients. Note templates speed documentation. It suits mental health and physical therapy. Updox centralizes tools. It adds fax, texting, and video in one spot. Practice management ties in. Providers manage multiple channels easy. ChARM Telehealth fits small practices. It offers e-prescriptions and billing. Patient portal shares summaries. Affordable plans keep costs down. AMC Health adds remote monitoring. Devices send data like blood pressure. Alerts flag issues early. Chronic care teams use it often. Secure Telehealth keeps things standalone. Video appointments run simple. Virtual waiting rooms organize flow. It works when EHR stays separate. PrognoCIS integrates telehealth with full records. Billing and management join. It suits clinics needing one platform. Kareo Clinical offers cloud ease. Telehealth fits with EHR and payments. Small practices adopt it fast. RXNT provides complete suites. Telehealth joins records and billing. Reporting helps track performance. These options cover various needs. Doxy.me wins for free start. Teladoc and Amwell lead for scale. Mend and SimplePractice suit focused care. Providers test demos to match workflows. Costs range from free tiers to custom quotes. Benefits show in more patients and less travel. Good software expands reach and improves outcomes.
Future Trends in Telemedicine Software
Telemedicine software heads toward more AI help. Tools will suggest diagnoses from symptoms. They pull past data for better advice. Voice notes turn speech to text fast. This cuts typing time. Remote monitoring grows with wearables. Devices track heart rate or glucose live. Alerts reach doctors quick. Integration with smart home tools adds context. Virtual reality aids physical therapy. Patients do exercises guided in 3D. Group sessions expand for support groups. Mental health benefits from shared spaces. Better video uses 5G for clear calls. No lag helps detailed exams. Blockchain secures data sharing. Patients control who sees records. Personalized portals show tailored health tips. Predictive analytics spot risks early.
Software flags potential issues from patterns. Mobile-first designs dominate. Apps work offline for basic entry. Global access improves with translation tools. Language barriers drop. Payment options add crypto or easy splits. Regulations adapt to new tech. Compliance stays built in. Hybrid models mix virtual and in-person. Software schedules both smooth. Data privacy gets stronger encryption. Cyber threats face better blocks. Training uses VR simulations. Providers learn fast. Partnerships link pharmacies for direct delivery. Labs send results instant. Telemedicine becomes standard care. It reaches underserved areas more. Costs drop as tech spreads. Providers adopt it for efficiency. Patients demand convenience. Future software focuses on access and outcomes.
Join Entri’s Hospital Administration Course
Conclusion
Telemedicine software changes healthcare delivery. It brings care to patients anywhere. Key features like video quality and secure sharing make it work well. Top options include Doxy.me for simplicity and Teladoc for scale. Providers gain from tools that fit their practice. Future trends add AI and monitoring for smarter care. Choose software that matches needs and grows with demand. Good telemedicine expands reach and improves results. It supports better health for more people. Start exploring options now to bring virtual care into daily work.
Frequently Asked Questions
What is telemedicine software?
Telemedicine software allows doctors and patients to connect remotely through video calls, messaging, and secure data sharing. It replaces in-person visits for many types of care. Patients join from home using a phone or computer. Providers use it to see patients without travel. It supports check-ups, follow-ups, mental health sessions, and urgent care. Basic versions provide video and chat. Advanced versions add e-prescriptions, payment processing, and file sharing. Most platforms keep conversations private with encryption. They follow privacy rules like HIPAA. Many connect to electronic health records for full patient history. Reminders reduce missed appointments. Rural patients reach specialists easily. Urban patients save time on travel. Providers see more patients daily. The software fits chronic conditions that need regular monitoring. It helps during bad weather or illness. Adoption stays high because it improves convenience and access. Patients like the ease. Providers report higher satisfaction. It bridges gaps in healthcare delivery.
Why do healthcare providers need telemedicine software?
Healthcare providers need telemedicine software to reach patients who cannot visit in person. It extends care to remote areas. It saves time for both sides. Patients avoid travel and waiting rooms. Providers fit more appointments into their day. The software reduces no-shows with reminders. It handles billing and payments directly. Secure messaging keeps follow-up talks private. Integration with health records gives doctors full information. This improves care quality. It supports chronic condition management without frequent office visits. Mental health services become more accessible. Providers cut office space costs. The tool fits busy schedules. It helps during emergencies or bad weather. Adoption grew fast and stays strong. Providers see better patient satisfaction. It meets modern expectations for convenient care. The software makes healthcare more efficient and inclusive.
What are the key features of good telemedicine software?
Good telemedicine software starts with clear video and audio for reliable consultations. No lag or drops ensure accurate exams. Screen sharing lets doctors show images or charts. Chat options allow quick notes during sessions. Waiting rooms keep patients organized. Scheduling tools make booking easy with open slots and reminders. Integration with electronic health records pulls patient history fast. E-prescribing sends medications directly to pharmacies. Secure messaging handles follow-ups privately. File sharing lets patients upload test results safely. Payment processing simplifies billing inside the platform. Patient portals provide access to records and summaries. Mobile apps support on-the-go use. Custom branding makes it feel like the clinic’s own tool. Multi-user support handles group sessions. Analytics track visits and outcomes. Security uses encryption and access logs. Compliance meets health rules. Easy setup avoids tech issues. Good support answers questions quickly. Scalability grows with the practice. Cloud options eliminate heavy hardware. These features make the software practical and safe for daily use.
Which telemedicine software is best for small clinics?
Doxy.me works best for small clinics. It runs in any browser without downloads. Patients join with one click. The free plan offers unlimited visits with basic HIPAA compliance. Paid plans add branding and group calls. Waiting rooms and chat keep sessions organized. Setup takes minutes. Cost stays low. It fits solo doctors and small teams. SimplePractice suits therapy and wellness clinics. It combines records, billing, and telehealth. Calendar syncs appointments. Secure messaging engages patients. Note templates speed work. It feels clean and easy to learn. Kareo Clinical offers cloud ease. Telehealth joins EHR and payments. Small practices adopt it fast. These options keep things simple. They avoid complex features small clinics do not need. Providers test demos to confirm fit. Benefits show in more patients and less overhead.
Which telemedicine software suits large hospitals?
Teladoc Health suits large hospitals well. It covers primary care, urgent needs, and specialties. 24/7 access connects patients anytime. Integration with health plans streamlines billing. AI tools triage cases quickly. Large networks use it for broad reach. Amwell scales for hospitals and systems. It links with records and devices. Remote monitoring tracks vitals from home. Behavioral health and chronic care get strong support. Custom workflows fit different specialties. Athenahealth Telehealth embeds into broader clinical platforms. Providers manage in-person and virtual visits together. Documentation, scheduling, and billing stay in one environment. These options handle high patient volumes. They support complex workflows. Security and compliance stay strong. Large hospitals benefit from scale and integration.
Is telemedicine software secure for patient data?
Telemedicine software stays secure for patient data. It uses encryption for all sessions. Connections protect information from start to finish. Platforms follow rules like HIPAA. Access logs track who views records. Secure messaging keeps follow-up talks private. Compliance tools meet health standards. Many vendors provide audit features. Patients control data through portals. Strong security reduces risks. Providers choose certified platforms. Regular updates fix vulnerabilities. Good software keeps data safe while allowing easy access for care. Patients trust it when privacy features work well.
How much does telemedicine software cost?
Telemedicine software costs vary by platform and size. Doxy.me offers a free plan with unlimited visits. Paid tiers start low for branding and extras. Teladoc Health and Amwell use custom pricing for large systems. Monthly fees range from hundreds to thousands. SimplePractice and Kareo start affordable for small practices. Cloud options keep upfront costs low. Some charge per provider or visit. Integration and support add to the price. Trials help test before paying. Benefits like more patients and less no-shows offset costs. Providers compare total value over time. Good software returns investment through efficiency and revenue.
Can telemedicine software integrate with existing systems?
Telemedicine software integrates with existing systems in most cases. Many platforms connect to electronic health records. Doctors pull patient history before calls. Billing tools link to practice management software. E-prescribing works with pharmacies. Remote monitoring devices send data directly. Integration reduces manual entry and errors. Care stays continuous. Vendors provide API connections. Some offer standalone options for separate use. Providers check compatibility during demos. Good integration saves time and improves workflow. It fits clinics and hospitals with current tools.